
One Teaspoon Of Salt Vs A Blood Pressure Pill
Emerging evidence suggests that cutting a single teaspoon of daily salt may lower blood pressure as much as a common hypertension pill by shifting renal sodium handling and vascular resistance.

Emerging evidence suggests that cutting a single teaspoon of daily salt may lower blood pressure as much as a common hypertension pill by shifting renal sodium handling and vascular resistance.

Emerging feline research suggests grooming, litter-box use, and sleep locations may reveal stress, pain and immune shifts more reliably than food, toys or visible mood.

A high snowy summit can place your phone’s GPS farther from Earth’s center than almost anyone else, showing that greatest altitude and tallest mountain are two different measurements.
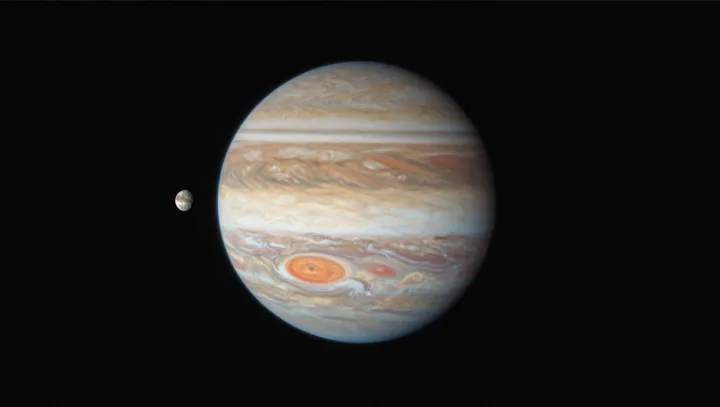
Jupiter’s Great Red Spot is shrinking while staying intense, revealing complex energy transport, turbulence and deep atmospheric dynamics beneath the visible storm.

Invisible odors plug straight into the brain’s limbic system, bypassing slower visual pathways and giving scent a unique leverage to reignite vivid, emotionally loaded memories.

Deadpool’s instant regeneration makes a sharp contrast with slow, tightly regulated human tissue repair, revealing why full organ or limb regrowth would break the rules that keep cancer in check.

Minimalist looks with one neon accent feel high fashion because they reduce cognitive load, heighten contrast, and trigger reward circuits for efficient visual processing.

Medieval stained-glass windows, built for religious storytelling, unintentionally functioned as early optical laboratories, experimenting with wavelength filtering, light scattering, and visual perception long before formal optics.

A bone-inspired luxury jewelry collection uses anatomy, entropy and material science to turn fragile biology into a visual argument about evolution, permanence and metamorphosis.

Explains how a soft paraglider wing becomes an efficient airfoil, using pressure, laminar flow and control inputs to ride rising air and stay aloft for hours.

Neuroscientists report that strenuous mountain climbs can trigger neural and hormonal states similar to deep meditation or short sensory deprivation, producing a shared sense of mental clarity and reset.